The intervention
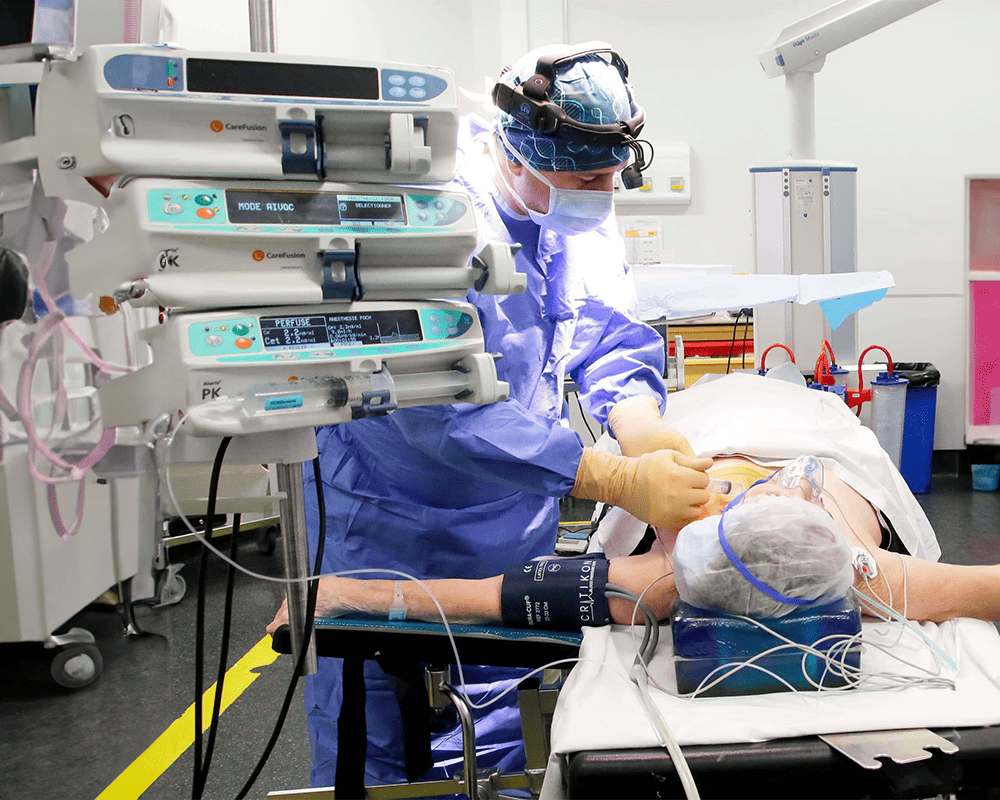
The intervention takes place under general anesthesia in the neurosurgery department, and lasts about 1 hour.
The neurosurgeon will make a small incision level with the neck to place small spring-shaped leads next to the left vagal nerve – as the right one can cause cardiac arrythmia.
A neurostimulator is implanted under the left collarbone.
The electrodes are hooked subcutaneously with the neurostimulator with electric wires.
The vagal nerve is a major structure of the nervous autonomous system which controls certain automatic physiological functions. It is the longest nerve in the organism.
It is divided into two parts (left and right): it starts off around the brain, goes down the brainstem into the neck, penetrates the thorax and takes the nerves out of many organs (the heart, the stomach, the digestive system, the lungs, the genital organs). That nerve plays a crucial role in the transmission of information from the brain to the body, and vice versa with the afferent fibers – which go from the periphery to the brain – and the efferent fibers – which go from the brain to the periphery. Therefore, with the vagal nerve, the brain controls thusly how organs function – which can, by themselves, send information to the brain about how they are doing, how they are working.
Vagal nerve stimulation consists in stimulating that nerve thanks to a small electrode implanted at neck level and hooked up to a small neurostimulation device: “a battery”.
Recommendations
Epilepsy
Epilepsy which either isn’t or is badly contained by medicated treatments is the first and most important reason for getting vagal nerve stimulation. Vagal nerve stimulation will be made available, if, like one epileptic patient out of three, your epilepsy is drug-resistant and that surgery is not possible – like in the case of an extended or multi-pronged epileptogenic outbreak – or fails.
Patient selection is made by the neurologists.
Vagal nerve stimulation consists of regularly (every 5 minutes, for example) sending brief and light electric pulses, via the vagal nerve, towards the cerebral areas associated with epilepsy, so as to help in controlling the electric disturbances which cause these seizures. That technique’s aim is not to cure epilepsy, but to reduce the frequency, the intensity, and the strength of these seizures. Studies also show improvements of mood, memory, and an increased vigilance. VNS (Vagal Nerve Stimulation) enables, as time goes by, a reduction in anti-epilepsy treatments and as such a reduction in their secondary effects.
That technique works both before seizures, and at the moment they happen, thanks to two additional devices:
- The magnet: you, or your loved ones, will have a magnet, given to you by your neurologist. You should start passing it in front of the stimulator, when you have a seizure, in order to kickstart a stronger and longer stimulation and make the seizure stop.
- An internal detection system: cardiac frequency picks up during a seizure. The generator can pick out that increased heart rate and kick start an additional stimulation. You do not have to intervene in that case.
Please note that VNS is a long-term stimulation: its efficiency is more notable over time.
Depression
Vagal nerve stimulation can only be offered in the case of some severe, chronic, drug-resistant depressions.
Clinical trials
The vagal nerve also has some anti-inflammatory properties, and some pilot-studies are currently taking place over use of its stimulation against certain chronic, inflammatory pathologies – inflammatory bowel disease (IBD), CROHN’s disease, rheumatoid arthritis, etcetera.