What you have to know
Spinal cord stimulation is a neurosurgical procedure which is made available when going through rebellious, chronic, drug-resistant neuropathic pain.
It is a reversible and lightly invasive technique. It is part of the patients’ global care and has the advantage of not inducing iatrogenic pain and limiting secondary effects. That approach’s success depends on different factors: the right patients being selected, which electrode is chosen and where it is placed, the settings, and, in the end, the patient’s therapeutic education, which plays a key role in that therapeutic therapy.
Concept
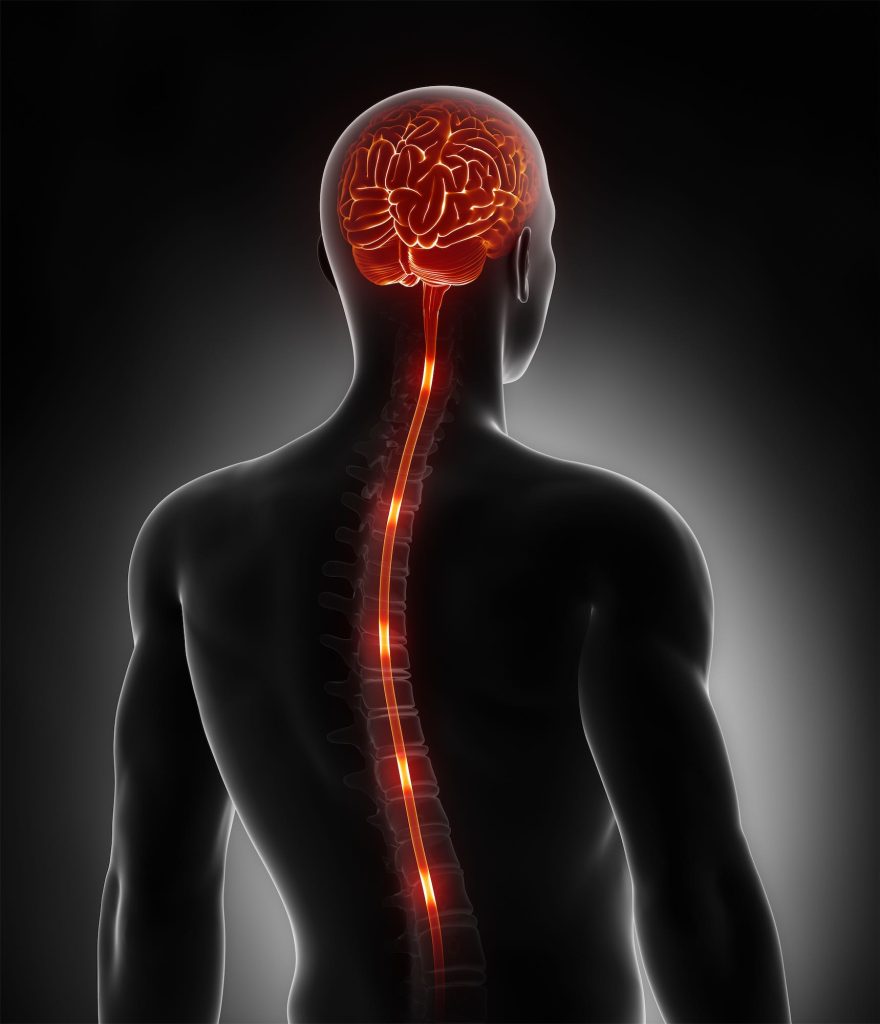
Spinal cord stimulation consists in sending out an electrical stimulation, in order to reduce pain, thanks to an electrode which is implanted near the bone marrow.
This neurosurgical technique directly acts on the systems involved in transmitting pain messages.
The electronic impulses scramble the pain signal, which the patient feels as painless paresthesia (tingling) in the areas which are usually painful.
Reasons for getting the operation
Spnial cord stimulation can be made available in case of chronic, drug-resistant neuropathic pain. That pain, described by patients as tingling, stinging, a painful sensation of cold, itching, allodynia, stabbing sensations, or even electrical shocks, is a pain which is secondary to a lesion or an illness which affects the somatosensorial system.
The most acknowledged reasons for getting the operation are refractory failed back surgery syndrome (FBBS) and Complex regional pain syndrome (CRPS Type 1 and Type 2).
- You might end up at the consult through a variety of ways:
- Your general practitioner;
- A specialist (rheumatologist, reeducation doctor, neurologist, orthopedist…);
- A center which specializes in pain management
An operability assessment takes place in a day-hospital. It includes a pain level evaluation, a neuropsychological evaluation, a cerebral and pan-medullar MRI scan, an SEP (somatosensory evoked potential) in order to evaluate the conduction of neural impulses on sensorial pathways, as well as a dental panoramic.
The advice to get that operation is given after the pluri-disciplinary staff’s decision (the staff generally consists with at least a neurosurgeon, an algologist and a psychologist) and depending on the results of the operability assessment. The advice is continued if your neuropathic pain is confirmed (with a DNA score > 4/10 ), if they date back at least a year, and if they are drug-resistant to well-lead treatments.
Furthermore, you must not present any cognitive disorders, any psychiatric disorders, or any personality disorders.
You are then informed of the staff’s decision. The team then defines goals with you, that should be doable if all goes well – as well as the modality of the operation and the pain management. It will be clearly pointed out to you that the intervention will not “cure” the disease, but only act against its symptoms.
An anesthesia consult takes place.
A consult with the treating nurse will be organized so that she can explain the two operating stages to you, and start off your PTE (Pre-operation Therapeutic Education).