What you have to know
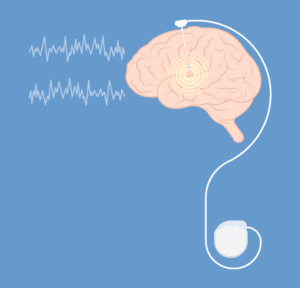
Deep brain stimulation (DBS) consists of implanting electrodes inside the brain in order to send it electrical impulses of both high frequency and low intensity.
That electrical stimulation will modify the operation of the networks of neurons whose activity has been modified by the illness.
Having Parkinson’s disease is the most common contra-indication of that neurosurgical technique.
Reasons to use it
Since it has been developed in France at the end of the 80s, many studies have proved both the efficiency of deep brain stimulation and the tolerance people have for it. Nowadays, it is used for many different reasons.
Parkinson’s disease
It is the most common contra-indication against deep brain stimulation. This technique does not cure the disease, but it does reduce its motor-symptoms – which are also called “dopa-sensitive” (tremors, rigidity, slowness) all the while decreasing the drug treatments.
However, that neurosurgical technique does not concern any and all diseases. You must, in order to benefit from it, correspond to well-defined criteria:
- Have been diagnosed of Parkinson’s disease according to its international criteria;
- Have an evolving disease for more than the last 5 years, in order to limit the risk of diagnostical errors concerning other parkinsonian-like disorders for which stimulation is contra-indicated (especially multiple system atrophy);
- Being under 70 years old (but the physiological age is mostly taken into account);
- To present a dopa-sensitive parkinsonian symptom which has improved of at least 50% on the motor-score of the MDS-UPDRS scale (Movement Disorder – Unified Parkinson’s Disease Rating Scale) after a Levodopa pharmacological test, since a significant dopaminergic reaction is a forerunner of the stimulation’s results;
- To be in general good health (progressive general diseases, or cardiac illnesses, or pulmonary, renal, haematological, ancerous, or an unstabilized diabetes);
- Do not present with important cognitive or psychiatric disorders.
A brain MRI can help rule out the cause being a lesion or vascular lesions, as well as eliminate anomalies which can point out atypical parkinsonian symptoms and evaluate the cortical atrophy in order to limit the risk of surgical complications.

One’s personal and social context is also taken into consideration in the final decision.
In the end, only 10 to 15% of all parkinsonian patients are concerned by this procedure, mostly those are afflicted by debilitating Parkinson’s disease. That debilitating aspect can be due to the persistence of great tremors which cannot be controlled by a well-lead drug-treatment, or due to the presence of motor complications of the dopa-therapy (fluctuations and dyskinesia).
One must note that recent studies have advocated for offering that surgery to young patients, who are still active, and whose motor handicap is limited, in order to limit the risk of negative socio-professional repercussions when the disease develops, but also to subjects who develop secondary psycho-behavioral effects when exposed to the dopaminergic treatments. We are then talking about precocious stimulation.
Chronic essential tremor
That genetic neurological disease makes up for the majority of abnormal movements, with one out of 200 people affected, with no distinction for gender. It can appear as soon as childhood and get worse over time, thus causing a real handicap for all daily life actions.
As of today, we do not know how to cure essential tremor or even curb its progression, but treatments have been developed that partially alleviate its symptoms, and as such better the quality of life of those it affects. They are, however, often disappointing and burdened by many sedative-like secondary effects.
If you arrive with a strong amplitude of abnormal movements – > 1 centimeter of range – deep brain stimulation will be offered to you. It is, in such a scenario, very efficient.
Dystonia
Dystonia results from agonist, antagonist and synergic muscular co-contractions – which can be sustained, brief, or lasting – and lead to abnormal postures and repetitive movements (tremors, myoclonic jerks, athetosis, …).
Dystonia’s origins can be monogenic genetics (in the case of pure or mixed dystonia), idiopathic, post-traumatic, peripheral (when there are neurogenic lesions or CRPS), postanoxic, postencephalitic, post-AVC (when the dystonia is belated).
There are several variations:
- Focal dystonia (blepharospasms, cervical dystonia, writer’s cramp, spasmodic dysphonia), segmented dystonia (limbs, trunk, head: Meige disorder), multifocal dystonia, hemidystonia or generalized dystonia;
- Permanent or paroxystic dystonia;
- Pure or mixed dystonia: myoclonic dystonia, spastic or ataxic dystonia…
The disease has its specificities:
- An antagonist gesture (which stops the symptoms):
- Context-specificity (action-wise: a musician, a golfer, a posture);
- An overflow (spreading in a limb).
The resistant focal or generalized forms of dystonia can respond efficiently to pallidal deep brain stimulation (that of the internal pallidus).
Other uses which are being studied
DBS is, in clinical research, being tested for other pathologies: severe treatment-resistant depression, Gilles de la Tourette disorder, obsessive-compulsive disorder (OCDs), mental anorexia, certain strains of pharmaco-resistant epilepsy, cluster headaches, etc.
A pluri-disciplinary decision for different target-areas
You will be chosen at the end of an comprehensive re-operation check-up which will be done by a pluri-disciplinary team (neurosurgeons, neurologists, neuropsychologists, neurophysiologists, psychiatrists, …). It includes a motor assessment, a neuro-cognitive check-up, a brain MRI, a psychiatric consult, a search for infectious hotbeds.
The electrodes will be implanted in specific areas of your brain, according to the pathology, the clinical results, your general health: sub-thalamic nucleus (STN), the internal globus pallidus, the thalamus. Those areas are defined unanimously by the pluri-disciplinary team.